Dr. Jonathan Schoeff, a physician specializing in longevity medicine and working with high-performance individuals, has a provocative message: cholesterol isn’t the enemy. He argues that many of the functions commonly blamed on “bad cholesterol” are, in fact, essential for health, repair, and resilience. Below is a closer look at what he proposes, and how it aligns (or conflicts) with current evidence.
Cholesterol in the brain: Structural support, not saboteur
Dr. Schoeff emphasizes that nearly 60 % of the brain is fat, and that cholesterol is a critical building block of neuronal membranes, synapses, and signaling. In his view, cutting cholesterol too low may undermine cognitive function, neuroplasticity, and repair.Indeed, scientific literature supports that cholesterol metabolism in the brain is tightly regulated, and disruptions can lead to neurologic disease. A review in EMBO Reports describes how defects in brain cholesterol homeostasis have been linked to Alzheimer’s, Parkinson’s, and Huntington’s disease.Additionally, a longitudinal study from China found that a long-term increase in total/non-HDL cholesterol was associated with slower cognitive decline, especially among women and those without cardiovascular disease.Still, the relationship is complex. A review of late-life cognitive decline noted that while midlife high cholesterol is often linked to dementia risk, in very old age higher cholesterol sometimes correlates with better cognitive scores.
Hormones depend on cholesterol as their precursor
Dr. Schoeff also emphasizes that cholesterol is the biochemical substrate for steroid hormones — from testosterone and estrogen to cortisol and aldosterone. In his view, overly aggressive cholesterol reduction can jeopardize energy, mood, libido, and endocrine balance.This is true: the body uses cholesterol (or derivatives) to produce steroids. While I did not find a definitive large trial showing that moderate lipid lowering causes hormone deficiency in healthy people, his point reinforces a principle many clinicians hold: lipid therapy should be balanced, and you don’t aim for zero cholesterol.
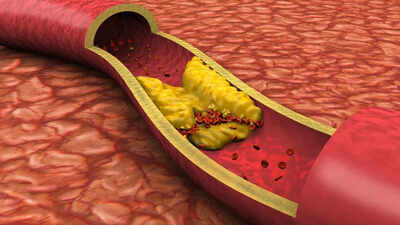
Cholesterol as the body’s repair crew
One of Dr. Schoeff’s boldest points is that elevated cholesterol may reflect a protective, restorative response, rather than pure pathology. He argues that cholesterol rushes in to help patch damage, especially following inflammation. From this view, the presence of high cholesterol should prompt attention to underlying causes (oxidation, metabolic stress), rather than reflexive suppression.This lines up, in part, with mechanistic theories. For example, cholesterol is integral to cell membranes, repair of lipid bilayers, and membrane trafficking. Some argue that in inflammatory states, more cholesterol is mobilized to heal tissues.

Yet, this doesn’t fully absolve high LDL from risk. Modified forms—oxidized LDL, small/dense LDL particles—are strongly implicated in atherogenesis and vascular inflammation. A review in BMC Medicine discusses the interplay of LDL, oxidation, and inflammation in cardiovascular disease.Aggressive LDL lowering, especially to very low levels, might have unintended effects on brain health, potentially increasing risks of cognitive impairment or dementia.Dr. Schoeff often states: “LDL isn’t one-size-fits-all.” He argues that the focus on total LDL-C is simplistic. What really matters are the subtypes (small, dense, oxidized), how insulin resistance and inflammation modify them, and how the body handles cholesterol traffic.Emerging evidence supports this nuance. A 2024 BMJ Open study found that lowest all-cause mortality corresponded to LDL-C levels in the range 100–189 mg/dL, which is much higher than often assumed.